The positives and negatives for the genetic, rare and undiagnosed community
During the Covid-19 pandemic all four nations have moved quickly to adopt remote consultations (either by phone or video) in order for patients to consult with healthcare professionals without risking exposure to the virus at clinics and hospitals.
In England, the Secretary of State for Health, Matt Hancock, underlined government support for telemedicine saying, ‘unless there are clinical or practical reasons, all consultations should be done by telemedicine’. Similar measures were also announced in Wales and Scotland. Scotland was perhaps better prepared as the NHS Near Me service has been developed for the Highlands and Islands – a video consulting service for clinical appointments which allows appointments to take place either at home or at a local NHS clinic.
In general practice the rollout has had mixed results. In Northern Ireland four out of 10 GPs have been unable to practise, while across the country seven out of 10 consultations were taking place online by the middle of April.
A great proportion of our genetic, rare and undiagnosed community need to avoid possible exposure to Covid-19 while requiring frequent consultations with healthcare professionals. As a result, these have become increasingly telemedicine consultations. The topic has been discussed both in our online forums and in our weekly community check-in call.
At this week’s community check-in, Kerry Leeson-Beevers, National Development Manager of Alström Syndrome UK, shared their experience of a switch to telemedicine at the Highly Specialised Service for Alström syndrome at Birmingham Children’s Hospital. This service would normally run 11-12 clinics a year, but all have been postponed since March and many local appointments have also been cancelled. In this context telemedicine clinics give families contact with experts and the assurances that this can bring, bridging the gap until clinics resume.
Alström Syndrome UK is developing a telemedicine information sheet with advice for what families could do to prepare for the appointments, helping families get used to the technology involved. They are also working on accessibility and translation services and attending clinics to support families. As an interim measure the remote consultations are clearly beneficial. Families were able to receive diet and nutrition advice, but it has not been possible to take blood to deliver the full range of tests that would occur in a face to face consultation, and many families do not have the equipment to take blood pressure or weight measurements at home.
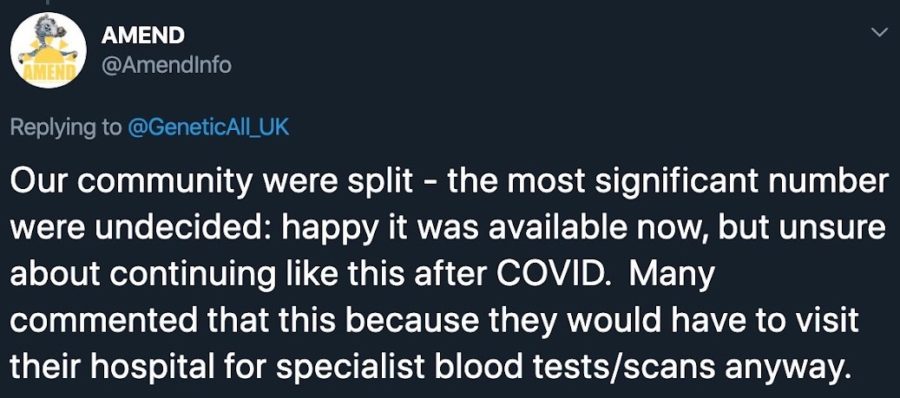
Remote consultations avoid challenging journeys, a plus for patients with mobility issues or for those who live far from their clinic, while helping them avoid the risk of travel-related exposure to Covid-19. For now, and during the pandemic, the consensus is in favour of remote consultations, but there are more mixed feelings about continuing remote consultations in the longer-term.
To make the most of the opportunities telemedicine offers, we must address all of the challenges.
While it is possible to deliver some types of ongoing care remotely, with some tests being possible provided families have the necessary equipment, full examinations, or initiating certain new treatments can’t be done remotely.
Patients and families need phones, computers and wifi for telemedicine appointments which not everyone will be able to afford or access. For some, sensory or cognitive disabilities may mean remote consultations are intrinsically more difficult or even impossible. As a result, telemedicine does not remove all barriers to accessing healthcare and some of the established ways of working through these. Some clinicians are reluctant to share test results over the phone, and building new relationships can be tricky, especially when a lack of nuance in remote communications hampers conversations. Such difficulties can be real barriers to delivering and receiving quality care.
Privacy and security are likely to become issues too, if the NHS does not get ahead of the risks and work hard to make sure both NHS staff and patients are doing all they can to avoid compromising the confidentiality of a health consultation.
Just as members of our community have been getting used to some of the benefits of telemedicine, we have heard that remote consultations have been cancelled and replaced by in-person appointments which, for some, is causing concerns as they are still shielding.
There are undoubtedly advantages to remote consultations, particularly where they supplement face-to-face consultations. But, we are learning from the Covid-19 pandemic experience that remote consultations for people living with genetic, rare and undiagnosed conditions cannot yet, and most probably never will, entirely replace the benefits of being physically in the same room as your healthcare professional.
For our community to benefit from this accidental telemedicine revolution, there will have to be recognition of the need to tailor services and that investment is needed to empower patients and enable access. Dialogue and flexibility from care providers will be crucial to embrace this opportunity.